Nurses and midwives trained outside the EU will be allowed to apply to come and work in the UK immediately after qualifying, following changes by the Nursing and Midwifery Council (NMC).
Until today nurses and midwives from outside the EU must have worked for at least 12 months after qualifying before being able to apply to work in the UK. The change brings applicants from outside the EU into line with their EU counterparts.
All those applying to work in the UK from outside the EU will still be required to pass the NMC’s stringent test to show they’re safe to work. They must also be able to show that they can communicate effectively in English.
The NMC has also introduced improved guidance and supporting materials for applicants so that they can be as well prepared as possible to show that they meet the regulator’s requirements.
These changes are part of a much wider ongoing review looking how the NMC can improve the experience for people applying to work in the UK from overseas.
Emma Broadbent, Director of Registration and Revalidation at the Nursing and Midwifery Council said:
“More than 65,000 nurses and midwives from outside the EU deliver first class care to millions of people across the UK every year and they are a vital part of our health and care workforce.
“This change will remove an unnecessary barrier, making it as simple and straightforward as possible for highly skilled nursing and midwifery staff to join the workforce.”
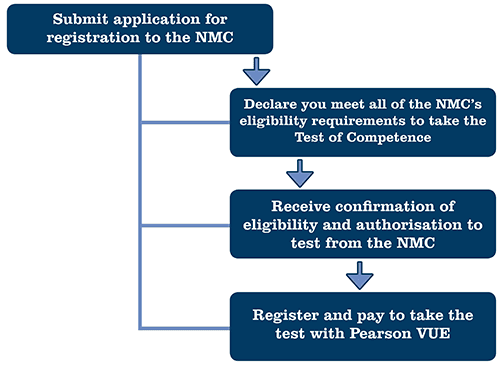
The Nursing and Midwifery Council (NMC), the professional regulator for nurses and midwives in the United Kingdom (UK) has approved the development and administration of a two part test of competence for nurses and midwives seeking registration in the UK.
The first of these tests is a computer based test (CBT) and can be undertaken at various Pearson VUE test and professional centers.

Nurses and midwives who have trained outside the European Economic Area (EEA) and want to work in the UK as a nurse or midwife must gain professional registration with the Nursing and Midwifery Council (NMC).
Applicants are tested for competence through a two-part process to gain registration.
- Part one - computer-based multiple-choice examination which is accessible around the world for applicants to access in their home countries.
- Part two - practical objective structured clinical examination (OSCE) which will always be held in the UK.
The immigration rules changed in March 2015 to allow for an individual nurse to come to the UK to prepare for the OSCE.
Rules for employers and overseas nurse applicants:
- All overseas applicants need to pass a computer-based test (CBT) and comply with all other initial requirements of the NMC overseas nursing process (including achieving language capability requirements) to be eligible to sit the OSCE and complete their registration. In October 2017, the NMC issued revised guidance on how an overseas applicant can meet the required level of English language capability.
- An individual entering the UK to take a nursing role has up to three months from the employment start date noted on the certificate of sponsorship (CoS) to sit the OSCE exam. During this period they can be legally employed as a pre-registration candidate.
- Employers must ensure that before a certificate of sponsorship is applied for:
- the individual has passed part one of the NMC test of competence
- the individual has been issued with an offer of employment, and
- the individual has achieved the required level of language capabiilty.
- In any applications for restricted certificates of sponsorship, you are required to send the following evidence to Tier2Limits@homeoffice.gsi.gov.uk
in support of the application:
- a copy of the employment offer letter
- a copy of the email confirmation from the NMC to show the individual has passed the CBT, and
- evidence that a Resident Labour Market Test (RLMT) has been carried out.
- The general Tier 2 minimum salary requirement of £20,800 is temporarily removed in these circumstances, though employers are still advised to place nurses in an interim position with a salary at least equivalent to that of a band 3 role.
- Applicants may sit the OSCE up to three times as part of one application (applies to applications started after 06 April 2017).
- If an applicant is unsuccessful at their first OSCE attempt, they must wait a minimum of 10 working days before they can take the examination again.
- If an applicant is unsuccessful at their second OSCE attempt, they must wait a minimum of three months from the date of their second attempt before they can take the OSCE for the third time.
- If the applicant is unsuccessful after their permitted attempts, the employer must stop sponsoring them and as a result their leave to remain period will be shortened.
- Upon successful completion of the OSCE and awarding of NMC registration, employers need to commit to ongoing employment of the individual as a registered nurse on a salary of at least £20,800.
- Employers must be able to provide evidence of the above arrangement if requested.
Employers or individuals with queries about individual NMC registrations are advised to contact the NMC directly.
Nursing included on shortage occupation list
Nursing was added to the shortage occupation list on 15 October 2015 but in a change to the rules, employers have been required to still carry out a RLMT before recruiting a non-EEA nurse from 24 November 2016. Find out more information in our Tier 2 policy changes section.
The continuation of nursing on the shortage occupation list means:
- applications for restricted certificates of sponsorship (RCoS) will be prioritised by the UK Visas and Immigration (UKVI) points allocation system - increasing the likelihood of nursing applications being granted
- the requirement to earn £35,000 or more to qualify for permanent settlement in the UK (indefinite leave to remain) will not apply to individuals for whom nursing has appeared on the shortage occupation list at any time during their employment in a nursing role - they will still need to meet all the other settlement criteria.
Applying for a certificate of sponsorship - need to know
- The first allocation panel to consider nurses as a shortage occupation was in December 2015.
- The Home Office has been clear that employers must only apply for certificates when you need them and when you are certain they will be used. The individual being sponsored must have a job offer from you and
either:
- have obtained full registration with the Nursing and Midwifery Council
- have passed the NMC's CBT of competence (part one)
- have obtained the NMC's permission before 30 April 2015 to undertake the overseas nursing programme, and be sponsored to undertake a supervised practice placement as part of the programme, which has been approved by the Nursing and Midwifery Council.
- You are required to provide evidence of the above in any applications for restricted certificates of sponsorship. You must send a copy of the employment offer letter and a copy of the email confirmation from the NMC to show the individual has passed the CBT. This evidence should be sent to Tier2limits@homeoffice.gsi.gov.uk to support your application.
We are still working within an overall cap of certificates. The inclusion of nursing is likely to have an impact on the success of other applications from health and other business, its therefore really important that we uphold these requirements from the Home Office to ensure we do not create a surplus of unused certificates.

The NHS is to hire 5,500 nurses from India and the Philippines in a desperate bid to plug staff shortages, health officials have said.
The mass recruitment exercise follows an increase in the number of UK graduates abandoning the profession, and a sharp drop in the number of nurses coming to work in Britain from the EU.
It comes as the Health Secretary sparked fury by signalling that reforms to NHS pay for nurses and midwives could be modelled along the lines of controversial changes to contracts for junior doctors.
Jeremy Hunt said a “more professional pay structure” was required for more than 1 million workers, who can currently get rates of up to 60 per cent more pay for weekend shifts....

Evidence from national data and partners
Nurses pass 5 of the 7 MAC top-down (i.e. national data) indicators of shortage. These cover employment, hours worked and skill shortage vacancies. There are also 3 pay indicators but these are not relevant at a time of pay freeze or severe public sector pay restraint.
The National Institute for Health and Care Excellence (NICE) guidance indicates that organizations should aim for a maximum 5% vacancy rate to accommodate operational flexibility needs. Health Education England (HEE), the body responsible for workforce planning for the NHS in England, estimates the current nurse vacancy rate in England at 9.4%, nearly double the NICE guideline. And in London, the RCN put the rate at 17%. Partner evidence suggests vacancy rates well above 5% in the care sector too.
Nurses’ pay accounts for about one tenth of NHS expenditure in England. In turn, spending on agency nurses is equivalent to one tenth of the nurse pay bill. Therefore, agency nurse spending – some 1% of NHS spending – should not be exaggerated. Nevertheless, such spending has risen rapidly in recent years. This is a further reflection of a nurse shortage.
National data and evidence from employers and trade unions therefore strongly suggests a shortage of nurses. Why?
Demand for nurses
Four main factors have boosted the demand for nurses in recent years. It is emphasised that the first three below should surely have been anticipated by those responsible for workforce planning:
- Population: the total population is rising and, in addition, people are
living longer and therefore require more nursing care;
- Reforms: moves to integrate NHS and social care, coupled with an
emphasis on 7 day working, raise demand;
Changing role of nurses: nurses have taken on more responsibilities,
including some duties previously carried out by doctors;
- Francis report and staffing guidelines: demand for nurses rose as
trusts sought to increase the nurse-to-patient ratios in response to the
2013 Francis report into events at Mid-Staffordshire NHS trust.